Out of Doctors, Out of Time: How to Build a Sustainable Healthcare Workforce
- America’s healthcare workforce is running on empty—and the provider shortage is about to hit crisis level.
- Burnout, budget cuts and red tape are draining the talent pool faster than new providers can fill it.
- Training programs can’t keep up—but creative investments in education, technology non-physician roles and technology could help turn the tide.
Feeling the squeeze
On the other hand, my nurse friend was coming home exhausted and overwhelmed every day from picking up slack due to staffing shortages. Then more of her colleagues resigned, and she absorbed their workload too. It wasn’t long before she followed suit.
A family member started experiencing crippling arthritis in her hands with signs of a possible autoimmune disorder. The first appointment she could get to see a rheumatologist or endocrinologist? Nine months out. There was nothing to do but cope and fume at the healthcare system.
You probably know someone in a similar situation. The shortage of providers brings enormous pressure and costs to the healthcare system for everyone, including consumers, providers and health insurance carriers. And it’s projected to get worse—alarmingly fast.
Here’s how to understand the precipitous healthcare workforce challenges we face and some creative ways to get some relief.
Don’t get caught lying down
You should be concerned about the current and worsening workforce shortage. What’s coming down the pike isn’t pretty.
Multiplying healthcare needs
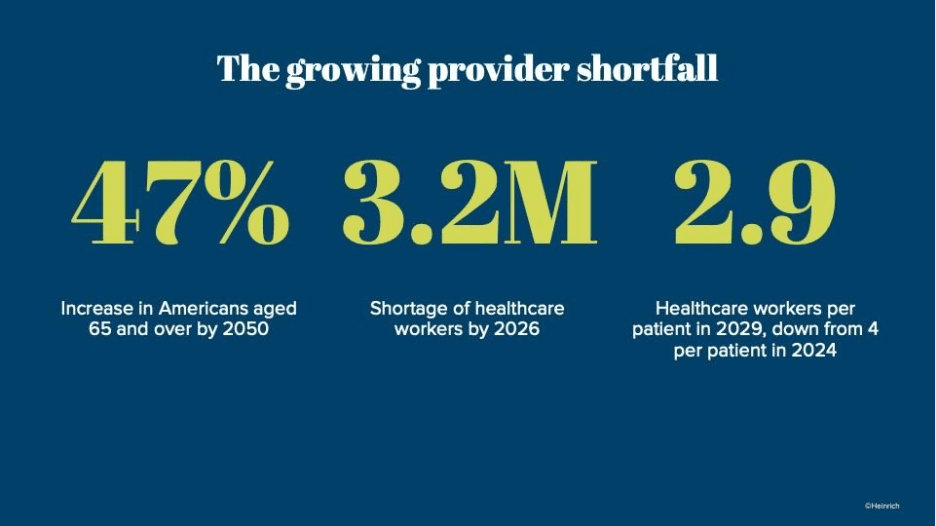
On the consumer side, we have an aging population. According to the most recent census in 2023, there were 55.8 million Americans aged 65 or older. This is projected to balloon to 82 million by 2050, a 47% increase. And as the senior population grows, the ratio of healthcare workers per senior could decline from four to only 2.9 workers per senior in the next five years.
Holes in the provider-workforce bucket
As the healthcare consumer population gets older, so does the provider workforce. Physicians who are currently 65 years or older make up 20% of the clinical physician workforce, while those aged 55–64 comprise 22%—adding up to nearly half of all physicians. Meanwhile, more than one quarter of nurses are expected to retire or otherwise leave the workforce by 2027.
With attrition putting more pressure on each healthcare worker, burnout is playing a main role in the reason providers of every age are leaving the field. In a vicious cycle, the turnover and shortages put a greater burden on the remaining workers, leading to further workforce departures. Although this trend peaked in 2022 during the pandemic and dropped for the first time since then in 2025, these factors continue to contribute to shortages.
All of this could hit especially hard in rural areas, which comprise 20% of the U.S. population but where only 10% of physicians practice for a number of reasons, mainly a lack of provider incentives. This is made worse by rural hospital closures, with 50% of rural hospitals operating in the red and potentially on their way to closure.
The trickling provider pipeline
In good news, medical school applications are up about 6% over the past five years. The number of newly licensed RNs is up 36%, supported by accelerated nursing programs that have nearly doubled the annual graduates over the past decade.
However, this represents a fraction of departures from the field and only slows down the worker shortage crisis. This is because significant challenges contribute to bottlenecks in the education and training of new healthcare workers.
- Experienced clinical faculty retiring faster than new educators can be recruited
- Retention hindered by burnout and emotional strain
- Financial, logistical and emotional barriers for students, especially from lower socioeconomic backgrounds
- Lack of scalability of apprenticeship-style, hands-on programs
- Persistent gaps in rural and behavioral health pipelines
- Investment and training challenges to leveraging outcome-improving technology

Photo by Erik Mclean on Unsplash
Coming up on a cliff
It’s projected that there could be a shortage of up 3.2 million healthcare workers by 2026 and of about 73,000 nursing assistants alone by 2028. This is alarming enough, but these projections were before a raft of potential changes in policy direction in 2025.
This is just a sampling of recent policy changes and impacts:
- CMS finalized a roughly 2.8% reduction to the 2025 Physician Fee Schedule conversion factor, potentially affecting Medicare participation and primary care capacity.
- A new $100,000 H-1B visa fee may affect the recruitment of international physicians, especially for rural and red-state markets that disproportionally rely on H-1B clinicians.
- Pandemic-era telehealth flexibilities face expiration in late 2025. If not extended, this could worsen access in shortage areas.
- Reorganization and reduction of the federal workforce by HHS could potentially delay programs and support functions that underpin workforce pipelines.
- States facing budget stress have begun cutting Medicaid provider payments even before federal budget changes take full effect, potentially limiting treatments and causing provider exits and service cutbacks in low-income and rural areas.
These policies could push shortages into an even steeper decline. Proactively preparing for the effects of these policies to be felt could save you from labor supply shock later.
Either ride the bike or fall off it
Healthcare as an industry faces a stark choice: address the provider shortage or spiral deeper into crisis. This calls for proactive, bold, coordinated and creative solutions.
Address the education and training bottlenecks
Training capacity is one of the biggest barriers to getting providers into the workforce. The industry will need to shift their perspective to long-term investment in more workforce entrants.
- Create funds to support and incentivize instructor and student recruitment and retention.
- Sponsor a faculty member, student cohort or apprenticeship program.
- Reduce the administrative burden of training center faculty and staff.
- Actively recruit, fund and provide emotional support programs for students with a lower socioeconomic background.
- Ramp up training in technologies that automate or improve education and training or create specialized technical support positions.
- Update regulations limiting the number of, or funding for, medical and nursing school residency slots.
- Provide programs for tuition forgiveness or scholarships.
- Expand training tracks from college to rural and underserved areas and specialties with workforce gaps.
Proactive support for these initiatives may need to expand from schools to clinics and hospitals to support their own future pipelines; meanwhile, local and state governments may need to step in to fill the gap not covered by the federal government.
Empower non-physician providers
Non-physician providers can help reduce administrative and care burdens for physicians, broadening access to care and freeing physicians up for the tasks requiring more training.
- Create more and accelerated training opportunities for non-physician practitioners.
- Adopt team-based care models where physicians supervise or collaborate.
- Expand scope-of-practice laws for nurse practitioners, physician assistants, pharmacists and midwives, especially in primary care and behavioral health.
These initiatives will require action by larger organizations and coalitions, either to reorganize training and care models or to lobby for policy change.

Photo by Vitaly Gariev on Unsplash
Shift the burden to technology
As technology, especially AI, advances in huge strides, shifting tasks from the pressured workforce to technology is vital. This is also one of the areas that providers have the most control over, whether you’re a large health system or an independent practice. Some of the many ways technology can bring relief:
- Administrative automation, intelligent staffing and scheduling: Relieve the administrative burdens that are a major factor in worker burnout.
- Recruitment support: Streamline finding, screening, interviewing, hiring and onboarding for hard-to-staff roles.
- Virtual assistants and chatbots: Handle patient intake, appointment scheduling and routine patient questions.
- Telehealth appointments and remote monitoring: Increase care capacity, especially in rural and underserved areas.
- Health, fitness, care and rewards programs: Provide free or low-cost support through phone apps or rewarding healthy activities monitored by smart wearables to help reduce the demand for care from healthcare workers.
These are just some of the ways technology is already helping workers improve outcomes more efficiently. Are you using them yet?
In the near future, AI will also likely be able to automate repetitive clinical tasks, support diagnosis, identify skill gaps, personalize training and forecast patient surges and supply bottlenecks. Staying at the forefront of technological advances may be one of the most accessible ways to start supporting the workforce now.
The highest-hanging fruit: policy reform
Many of the most impactful solutions require policy reform, which is frustratingly out of our control. However, if there’s any hope of influencing policy, proactively organizing today is the key to laying the foundation for policy reform tomorrow. For those changes that do require policy reform, different parties in the industry may need continue to form broad coalitions to lobby for policy measures that benefit providers, carriers and consumers alike.
Make the pivot
This isn’t just a staffing issue. It’s a turning point for the entire healthcare system. The organizations that move first—automating where they can, investing in people where they must and reimagining care delivery—will define the next era of healthcare. The question isn’t whether the shortage will shape your business. It’s whether you’ll shape what comes next.
Have you felt the impacts of the provider shortage yet? What do you see as the way forward? We’re here to help you transition to new ways of managing workforce and access to care. Get in touch today.

